Unveiling the power of visuals: Exploring top Gliffy alternatives for diagramming
Diagramming is a powerful method that goes beyond just drawing lines and shapes. It allows teams to map out complex processes, brainstorm new ideas, and communicate complex systems simply and effectively. As businesses face increasingly complex challenges, the ability to visualize these issues is crucial. Diagramming tools have come a long way, from basic drawing utilities to comprehensive platforms that enable collaboration, integration, and scalability across various business functions. The right tool can help break down barriers between remote teams, foster understanding across different departments, and even help strategize business growth. This article will help you navigate the busy landscape of diagramming tools, starting with an in-depth look at Gliffy and its many alternatives to help you determine which tool best suits your team's needs.
Deep dive into Gliffy: Evaluating a key player in diagramming
Gliffy has made a name for itself as a versatile diagramming tool that integrates effectively with other enterprise systems, particularly those in the Atlassian suite like Confluence and JIRA. Teams often choose Gliffy for its user-friendly interface that makes creating complex diagrams approachable for team members of any skill level, and it's favored for its seamless integration and ability to enhance documentation with clear visual aids.
Here are some Gliffy features:
Drag-and-Drop Interface: Simplifies the creation of diagrams, making it accessible even for those who aren't tech-savvy.
Collaboration Tools: Allows multiple users to edit and comment in real time, facilitating teamwork.
Integration with Atlassian Products: Enhances workflows by connecting diagrams directly to projects and documentation in Confluence and JIRA.
Template Library: Offers a variety of pre-made templates that can kick-start the diagramming process and inspire users.
Exploring Gliffy alternatives: Why your team might need different diagramming solutions
While Gliffy is a popular choice for online diagrams, your team's unique needs might call for different features. Various diagramming tools offer specialized functionalities that cater to specific project requirements and team dynamics, such as advanced collaboration features, extensive shape libraries, or seamless integration with other platforms. Considering alternatives to Gliffy can help your team find a more tailored, cost-effective solution that boosts productivity and enhances creativity. Let’s look at some popular options that could better align with your workflow.
Top 10 Gliffy alternatives
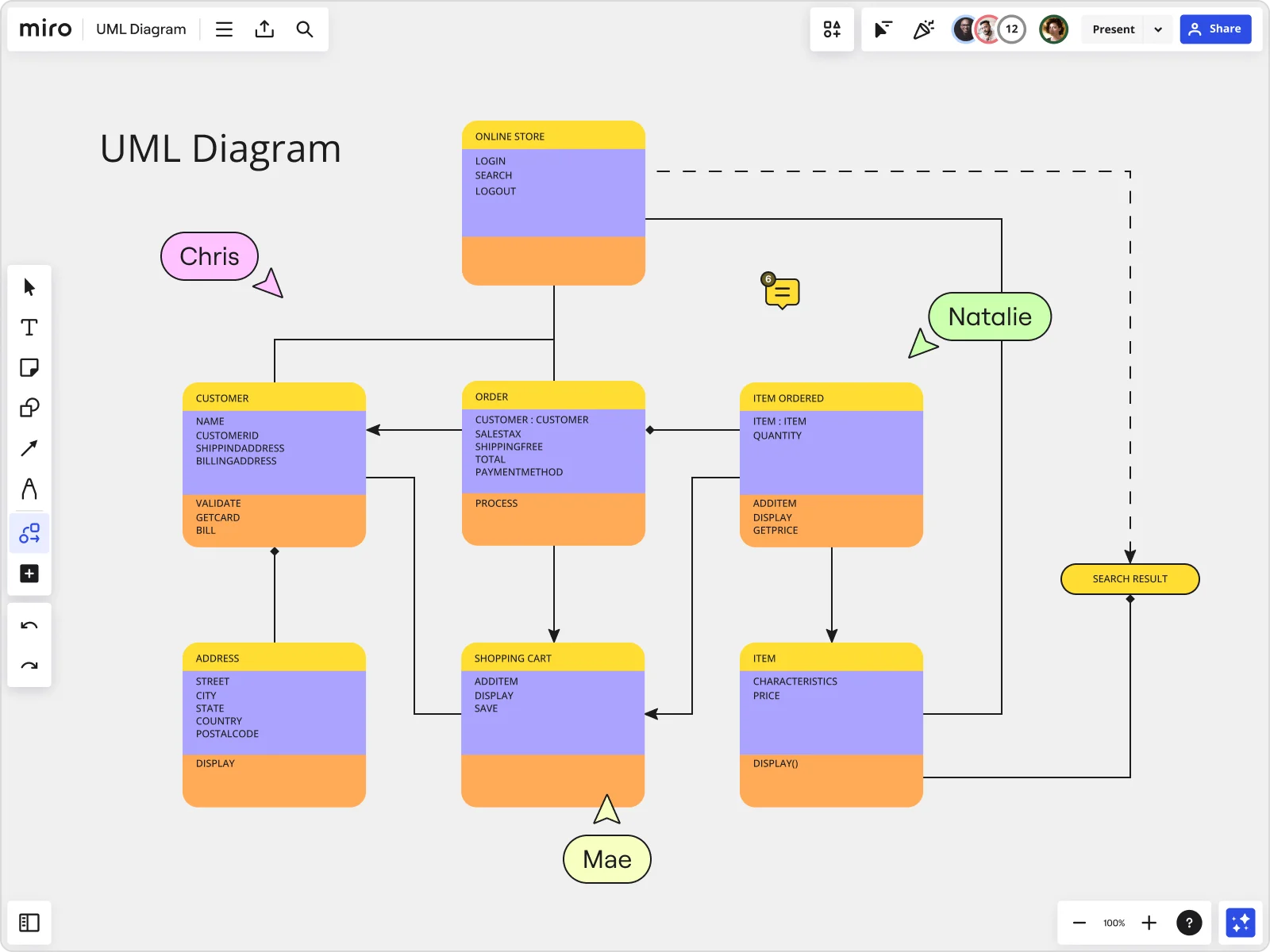
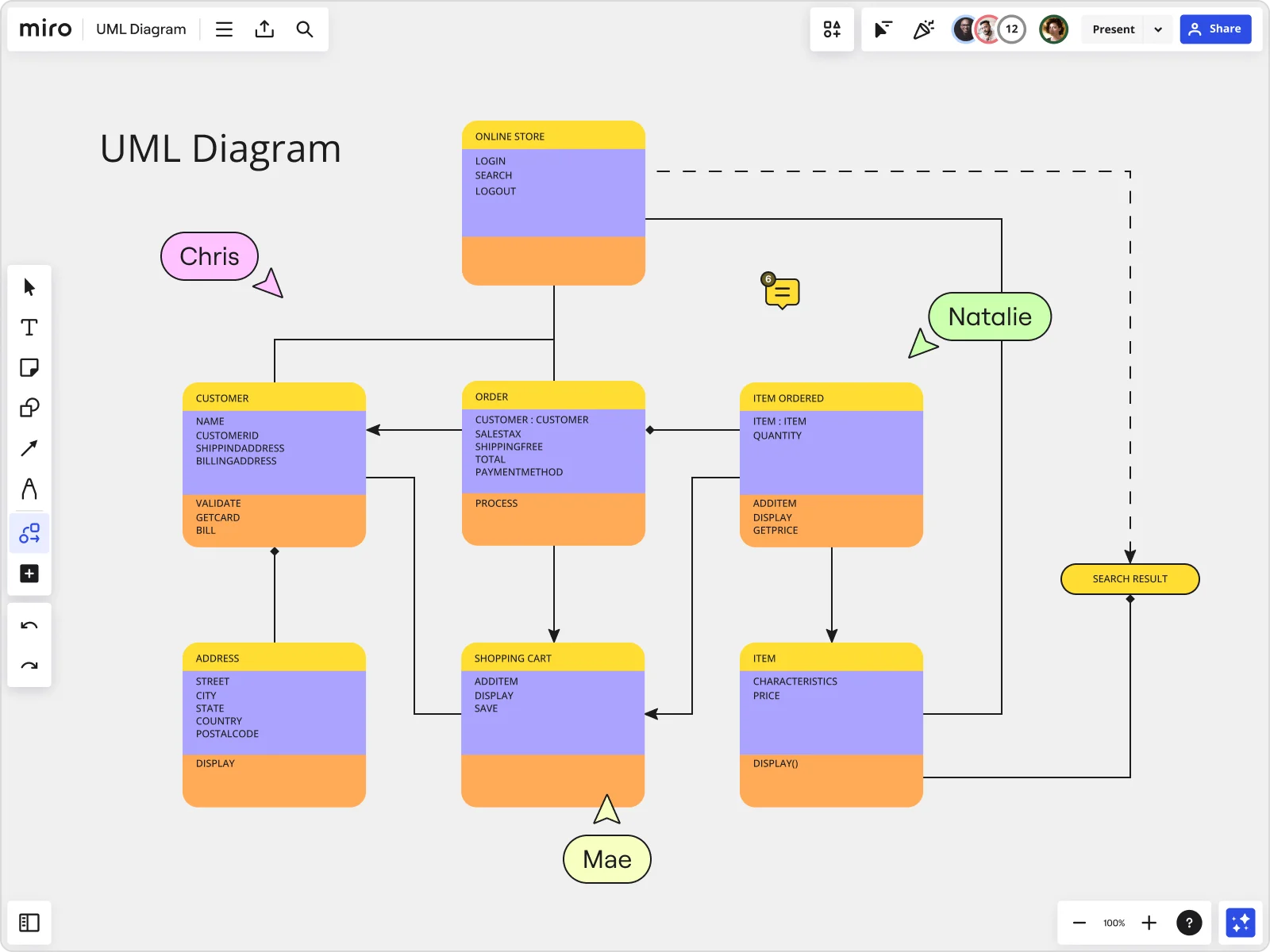
Miro
Miro is an interactive workspace designed to bring teams together no matter where they are located. Its comprehensive set of tools supports not just diagramming but also brainstorming and project planning, making it a multifunctional workspace.
Miro is especially popular among teams that require a high level of collaboration and flexibility in their tools. Dynamic design, software development, and project management teams looking for an all-in-one workspace.
Features:
Infinite Canvas: Provides limitless space for brainstorming and mapping complex workflows.
Real-Time Collaboration: Enables team members across different locations to work simultaneously on the same board.
Extensive Integrations: Works with apps like Slack, Asana, and more to keep all tools in one place.
Interactive Templates: Offers ready-to-use templates that cater to various needs and industries.
Pros:
Unmatched for collaborative diagramming with tools that support a highly interactive environment.
Extensive customization options make it adaptable to a wide range of use cases.
Supports a broad array of integrations, enhancing its utility within different technological ecosystems.
Cons:
The array of features and expansive environment can be overwhelming for new users or those with simpler needs.
Dependence on a strong internet connection for optimal performance, which can be a limitation in low-bandwidth areas.
Lucidchart
Lucidchart is a tool that enables the creation of professional diagrams essential for process modeling and data visualization. Its appeal lies in its flexibility and the depth of features offered.
It's ideal for teams that need robust, secure, and scalable diagramming capabilities and large enterprises or tech teams that require detailed workflow documentation and process diagrams.
Features:
Collaborative Workspaces: Supports simultaneous editing and commenting by multiple users.
Extensive Shape Library: Comes equipped with a wide range of shapes and connectors to suit different diagramming needs.
Dynamic Data Linking: Users can connect diagrams directly to live data for automatic updates.
Secure Cloud-Based Platform: Ensures that data is safe and accessible from anywhere.
Pros:
Advanced collaboration tools enhance team interaction and diagram accuracy.
Strong integration capabilities streamline workflows across various platforms.
Rich feature set suitable for both simple and complex diagramming needs.
Cons:
May be too complex and feature-rich for users who need basic diagramming capabilities.
The cost can be a barrier for smaller teams or individuals.
Creately
Creately is known for its versatility, providing a platform that is not only great for diagramming but also excels in creating mind maps and project visuals. Teams chose it because of its dual project management and visual documentation functionality.
Features:
Visual Project Management: Integrates diagramming with task management to enhance project visualization.
Real-Time Collaboration: Allows team members to collaborate on diagrams in real time, improving team alignment and decision-making.
Diverse Diagram Types: Supports a wide range of diagrams, from simple flowcharts to complex network diagrams.
Pros:
Flexible tool useful for multiple project types.
Affordable pricing makes it accessible for smaller teams.
User-friendly interface suitable for both technical and non-technical users.
Cons:
Limited customization options in the free version.
Performance can lag with very large diagrams.
Visio
Microsoft Visio is a powerful diagramming tool favored by professionals that requires precision and advanced functionalities, especially in IT and engineering. People appreciate its comprehensive features and seamless integration with other Microsoft products.
Features:
Advanced Diagramming Tools: Offers specialized tools for creating detailed network layouts, floor plans, and engineering designs.
Data Linking: Can link diagrams directly to data sources to display real-time information.
Wide Range of Templates: Provides a vast library of pre-designed templates that cater to various industries.
Pros:
Highly detailed and precise diagramming capabilities.
Strong integration with Microsoft Office suite.
Suitable for large organizations with complex diagramming needs.
Cons:
Higher cost barrier compared to other options.
Can be complex for beginners or those with basic diagramming needs.
Sketch
Sketch has made a name for itself primarily in the design community, focusing on UI/UX design tasks, but it has also proven effective for creating wireframes and prototypes. It's a popular tool among design teams for its specialized tools in high-fidelity visual design.
Features:
Vector Editing: Allows precision in creating and editing scalable vector graphics.
Plugin Ecosystem: Extensive range of plugins available that extend functionality and workflow.
Collaboration Tools: Facilitates sharing and feedback with tools designed for design teams.
Pros:
Focused on design, offering tools that are highly beneficial for UI/UX projects.
Great for creating prototypes that can be passed directly to developers.
Supports an active community with numerous third-party plugins and resources.
Cons:
Primarily suitable only for macOS, limiting accessibility.
Not as versatile for non-design tasks, such as general business diagramming.
EdrawMax
EdrawMax offers extensive diagramming capabilities with support for over 280 types of diagrams, making it a flexible solution for virtually any visual task. Some teams choose it for its comprehensive tools that cater to various diagramming needs across different fields.
Features:
Extensive Diagram Types: From flowcharts and mind maps to complex engineering schematics.
Templates and Symbols: Provides many templates and symbols to speed up the diagramming process.
Cross-Platform Support: Available on Windows, Mac, and Linux.
Pros:
Wide range of features makes it suitable for many different types of professional use.
Affordable pricing with a flexible licensing model.
User interface is intuitive, making it accessible to all skill levels.
Cons:
Some users may find the interface outdated compared to newer diagramming tools.
Occasional bugs and performance issues with more complex diagrams.
Cacoo
Cacoo is a cloud-based diagramming tool that facilitates real-time collaboration across teams, making it a great choice for projects requiring frequent updates and team input. Favored for its collaborative features and ease of use, teams use it when they need a straightforward, no-frills approach to diagramming with a strong emphasis on teamwork.
Features:
Cloud-Based Collaboration: Enables multiple users to work on diagrams simultaneously from anywhere.
Integration Capabilities: Integrates with cloud storage solutions like Google Drive and Dropbox.
Template Library: Offers a variety of templates to help teams get started quickly.
Pros:
Simple and intuitive interface.
Real-time collaboration encourages team participation.
Affordable with various subscription options.
Cons:
Limited in terms of customization and advanced features.
Mainly suitable for simpler diagramming tasks rather than complex technical diagrams.
Figjam
Figjam, part of the Figma design ecosystem, offers a focused and modern approach to collaborative diagramming, especially suitable for design-oriented teams. It's the go-to for creative teams that need a tool that supports the fluid transition between design and diagramming.
Features:
Seamless Figma Integration: Works smoothly with Figma, maintaining consistency across design and diagramming.
Interactive Elements: Tools like sticky notes and voting help facilitate dynamic brainstorming sessions.
User-Friendly Interface: Designed to be intuitive and easy to navigate for designers.
Pros:
Excellent for design-focused diagramming.
Encourages collaboration with easy-to-use communication tools.
Fresh, modern interface that appeals to creative teams.
Cons:
As a newer tool, it may lack some advanced features found in more established diagramming platforms.
Best when used in conjunction with Figma, which might limit its use to primarily design tasks.
SmartDraw
SmartDraw is recognized for its automated diagramming capabilities, which simplify the creation of professional-grade visuals with minimal effort. Teams choose it for its ability to automate complex diagramming tasks, saving time and effort.
Features:
Automated Formatting: Automatically adjusts and aligns diagrams for a professional finish.
Massive Template Selection: Extensive templates collection covering a wide range of industries and use cases.
Integration Options: Supports integration with tools like Microsoft Office, Google Workspace, and more.
Pros:
Reduces the time needed to create complex diagrams.
Ensures consistency in diagram aesthetics and structure.
Offers extensive support and resources for new users.
Cons:
Premium features come at a higher price point.
Automation can sometimes reduce flexibility in design options.
Draw.io
Draw.io (now known as diagrams.net) is a robust, open-source diagramming tool favored for its no-cost access and straightforward functionality. Teams use it for its cost-effectiveness and straightforward approach to diagramming without unnecessary complexities.
Features:
Open Source: Free to use with access to its source code for customization.
Integration with Collaboration Tools: Integrates seamlessly with Google Drive and Confluence.
Wide Range of Diagram Types: Supports a vast array of diagram types, suitable for various professional uses.
Pros:
Completely free, making it accessible for startups and non-profits.
Simple user interface that is easy to navigate.
Suitable for technical and non-technical users alike.
Cons:
Lacks some of the advanced features and support provided by paid alternatives.
The user experience may not be as polished as that of more modern tools.
What now? Diagram with confidence
Choosing the right diagramming tool can be pivotal for team collaboration and productivity. Each tool offers unique features that cater to various team dynamics and business needs. When making a decision, consider the following:
Integration Needs: How well does the tool integrate with your current tech stack?
Usability: Is the tool easy for everyone on your team?
Customization: Can you tailor the tool to fit your project requirements?
Collaboration Features: Does the tool support the level of collaboration your team needs?
Miro emerges as a solid candidate for teams aiming to innovate and streamline their workflow. It supports diagramming and enriches the process with tools for project management, collaborative brainstorming, and seamless integration with many other platforms. This makes it an excellent choice for teams looking to push boundaries and elevate their visual communication to the next level. Harness the power of diagramming and choose a tool that best fits your team's ambition and style.